Keep Your
Hamster Healthy
Hamsters are one of the most popular small pets around the world. They are cute, cuddly and friendly, making them an ideal family pet. These tiny creatures are known for their energetic nature and fast-paced movements, which can bring joy and excitement to any household. In this blog post, we will be discussing everything you need to know about hamsters, from their diet and habitat requirements to their behavior and proper care.
Whether you’re a seasoned hamster owner or a curious beginner, this guide will provide you with all the information you need to ensure your furry friend lives a happy and healthy life. Let’s dive in! Here is a recap for our Hamster Blog:
- Research popular topics related to hamsters such as care, nutrition, and behaviors.
- Choose a domain name for the blog and purchase hosting.
- Install a content management system (e.g. WordPress) on the hosting.
- Choose a theme that is visually attractive and suitable for a blog about hamsters.
- Create content for the blog such as articles, videos, images, polls, and other interactive elements.
- Market the blog on social media and other platforms to attract readers.
- Create a mailing list for users who want to be notified about updates to the blog.
- Establish yourself as an authoritative source by providing accurate information about hamsters and regularly updating content.
- Respond to reader feedback to build a relationship with followers and encourage repeat visits.
- Analyze user data to discover popular topics and adjust content strategy to focus on those topics.

An Overview of Species and Traits: Syrian Hamster | Teddy Bear
Hamsters are adorable, small rodents that make popular house pets. As members of the biological order Rodentia, they are distant relatives of mice and rats. There are 19 species of hamsters, belonging to the subfamily Cricetinae and classified into seven different genera. The Syrian hamsters or golden hamster, Mesocricetus auratus, is the most common species and comes in a variety of coats, including the long-haired or Teddy Bear breed. Hamsters are known for their short tails and stubby legs, with adult body lengths ranging from 50 mm to 340 mm.
They are small animals that come in a variety of colors such as black, brown, gray, white, yellow, or red. With their fluffy and cute characteristics, hamsters are a delight to watch as they play and self-groom. Understanding hamster species and traits is essential for choosing the right breed as a pet, handling and bonding, providing the appropriate housekeeping, diet, and nutrition to keep them happy and healthy.

Choosing the Right Species: A Guide to Popular Breeds for Pets
When it comes to choosing a pet hamster, there are several different species to consider. The most popular breed for pets is the Syrian or Golden Hamster, known for their docile and friendly personalities. Chinese and Dwarf hamsters are also common choices, each with their own unique traits and characteristics.Also available in your nearby pet stores.
Before making a decision, it’s important to research each breed and consider factors such as size, activity level, and recommended care requirements. With the right breed and proper care, a hamster can make a happy and beloved addition to any family.
Understanding Behavior: From Solitary Habits to Aggression
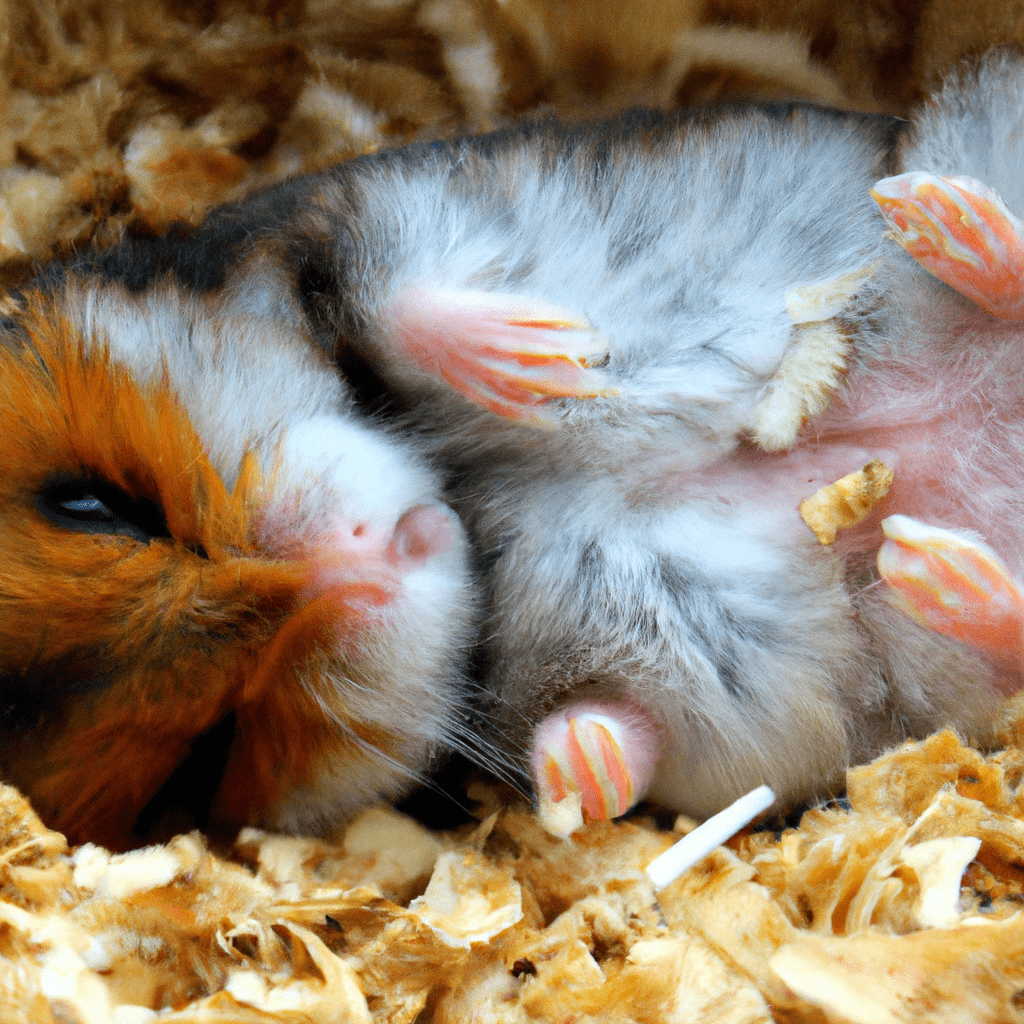
In order to keep your hamster healthy and happy, it’s important to understand their behavior. Hamsters are solitary animals by nature, which means they prefer being on their own. Syrian hamsters, in particular, are known to be territorial and may not tolerate other hamsters in their cage. On the other hand, dwarf hamsters may tolerate siblings or same-gender unrelated hamsters if introduced at an early enough age, but this cannot be guaranteed.
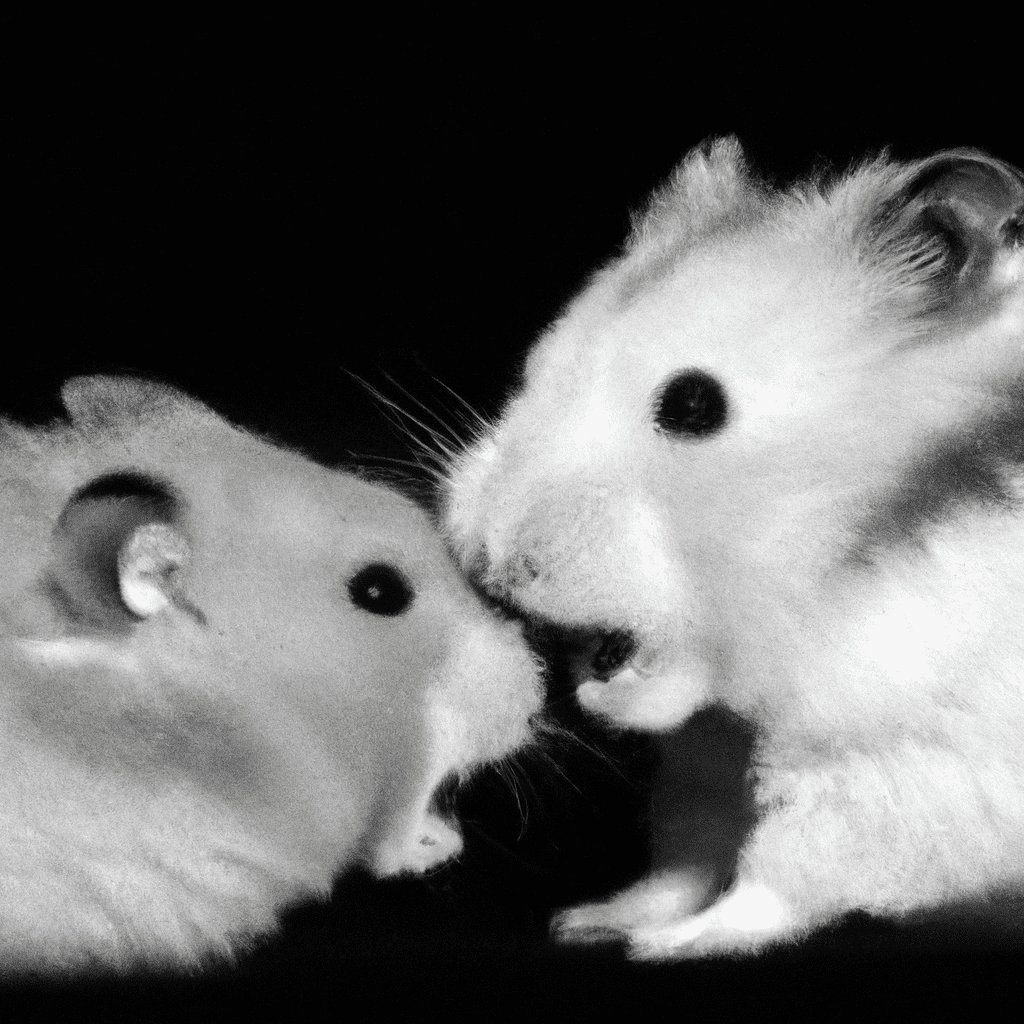
It’s important to note that hamsters can also display a range of emotions, including being happy, afraid, threatened, curious, startled, angry, and more. Additionally, female hamsters exhibit high rates of territorial aggression in adulthood, as compared to males. By keeping this information in mind, you can provide a safe and comfortable environment for your hamster and avoid any potential aggression or territorial behavior.
Food ,Diet & Nutritional Requirement
When it comes to feeding your hamster, it’s important to remember that they are omnivores and need a balanced diet of both plants and protein. While their natural diet consists of grasses, seeds, and grains, it’s important to supplement this with fresh greens, fruits, and vegetables to ensure they get the vitamins and minerals they need.
Simply feeding them seeds will result in nutritional deficiencies in vitamins and minerals, specifically vitamin E and calcium. Pellets are not necessary for their diet, but a mixture of different seeds formulated to meet their needs is recommended. Additionally, hamsters need access to fresh, clean water at all times. By providing your hamster with a balanced diet and proper hydration, you can help keep them healthy and happy.

Care and Feeding Requirements: How to Keep Your Pet Healthy and Happy
Taking care of a hamster’s dietary needs is crucial to keeping them happy and healthy. Providing them with a balanced diet of pelleted food, fresh vegetables, and occasional treats will ensure that they get the necessary vitamins and minerals. It’s also important to provide access to clean water at all times. Regular exercise is also essential for the maintenance of their wellbeing, just like any other pet.
Hamsters need plenty of opportunities to explore and play, so it’s important to create an enriching habitat that allows them to climb, run, and burrow. Keeping their living space clean and comfortable is also vital for their health and happiness, as an unclean cage can lead to various health issues. By following these care and feeding requirements, hamsters can live a fulfilling life as your furry friends.
Common Health Concerns: How to Spot and Treat Common Diseases
As with any pet, hamsters can face health concerns from time to time. It’s important to be aware of the signs of common hamster diseases so that you can spot them early and seek treatment. Signs of infection can include diarrhea, dehydration, weight loss, rough hair coat, and a swollen or bloated abdomen. Hamsters can also develop ear infections or abscesses, which can be painful and require veterinary attention.
Other common illnesses include Wet Tail Disease, fungal infections, lip scabs, diarrhea, cold virus, and mite infestations. By keeping an eye out for these symptoms and seeking professional care as needed, you can help ensure that your furry friend stays healthy and happy. And of course, regular check-ups with a veterinarian can help prevent health problems before they occur.
Hamster Diagnostic Testing Services
Testing offers testing services for pet hamsters to detect any potential health issues. Tests include blood work, X-rays, and other examinations to check for diseases, parasites, and other complications.

Hamster Cage Type,Setup ,Maintenance & Safety Issues
When it comes to setting up a home for your furry friend, it’s essential to consider the type of cage that will best suit your hamster’s needs. Plastic, wood, ready-to-use, and glass tanks are all options, each with their pros and cons. While hamsters seem to prefer cages with bars, avoid using wood due to potential odors and fear factor. Glass tanks can also cause distress if they overheat, so proper placement is crucial.
Regardless of cage type, it’s important to clean it thoroughly at least weekly and provide fresh bedding, food, and water daily. Hamsters also need ample floor space, with height being less of a concern. It’s important to handle your hamster with care when returning them to their cage, and be mindful of potential injuries from falls. By creating a comfortable and safe habitat, you can help ensure your hamster stays healthy and happy.

Creating the Perfect Habitat: Tips for Setting Up Your Pet’s Home
Creating the perfect habitat for your hamster is essential for their health and happiness. As mentioned earlier, hamsters need a quiet and calm area of the house to feel comfortable. It’s also important to provide them with enough space to play, climb, and exercise. Choose a cage that’s as large as possible, with several levels and hiding places for your hamster to explore. To keep your hamster healthy, maintain a clean and dry cage, and change their bedding regularly.
Additionally, consider offering your furry friend some playtime outside their habitat each week. Remember to place their cage in a location with no loud noises or vibrations as this could cause stress to your pet. Lastly, add a structure to the cage for your hamster to store food and hide in. By following these tips, you’ll be well on your way to creating a perfect habitat for your hamster.

Handling and Bonding: Building Trust with Your Hamster
As any hamster owner knows, building trust with your furry friend takes time and patience. In this section, we’ll explore some helpful tips and techniques to help you and your hamster bond. Start by allowing your hamster to climb on you, so they become familiar with your scent. Make sure to speak quietly and avoid sudden loud noises or movements, as hamsters can be easily startled. Offer small treats to encourage interaction, and be patient as your hamster gets to know you.
Remember that each hamster is unique, so take your time getting to know their personality and preferences. With consistent effort and affection, you can build a strong bond with your hamster that will bring joy for years to come.
:strip_icc()/GettyImages-1206094142-4ea14976f93f4600a0b00010f93487d9.jpg)
Hamster Playtime: Fun Activities to Keep Your Pet Active and Engaged
After you’ve set up a perfect habitat for your hamster, it’s time to give your furry friend the playtime he deserves! To keep your pet active and engaged, there are plenty of fun activities you and your hamster can enjoy together. Try creating a cardboard tube maze or obstacle course, which can provide hours of fun for your hamster as they love burrowing and exploring.
Running wheels are also a favorite activity for hamsters, as they help them get their daily exercise. In addition to these activities, engaging in one-on-one playtime with your hamster can also help build trust and create a stronger bond between you and your pet. Remember that playtime is an essential part of your hamster’s daily routine, and by providing them with various activities, you can keep them healthy and happy.

Toys Types, Safety Materials & Maintenance
Hamsters are active and curious creatures that need various toys and hamster ball to keep them entertained and exercised. From chew toys to tunnels, there are several types of toys available that are safe for hamsters to use. Wooden toys are a good option as long as they are pesticide and chemical-free, while barred and meshed wheels must be avoided as small paws can easily fall through the gaps.
Safety materials are also crucial when it comes to hamster toys, as they can easily slip and fall, leading to potential injury. Regular maintenance of toys is also important to prevent any hazards or damage. Providing a range of safe toys is a great way to keep hamsters healthy, active, and mentally stimulated.
Lifespan
Hamsters can live up to 2-3 years on average, but in some cases have been known to live up to 4 years. However, this can depend greatly on the type of hamster that you have. Syrian hamsters have the longest lifespan, usually ranging from 2-3 years. Dwarf hamsters, such as Russian and Chinese, usually have a shorter lifespan of 1-2 years. Roborovski hamsters are known to have the longest lifespan of all, sometimes living up to 4 years old.
It is important to give your hamster good care in order to make sure that it lives a long and healthy life. You should provide your hamster with an adequate amount of food, water, and exercise. Make sure that the cage that your hamster is kept in is cleaned regularly, and that the bedding is replaced at least once a week. Additionally, make sure to provide other items such as toys, chew sticks, and climbing toys to keep your hamster entertained and active.
Proper nutrition is also important for a hamster’s health and longevity. It is important to provide your hamster with a balanced diet made up of fresh vegetables, fruits, grains, and animal-based proteins. Hamsters should also always have access to fresh, clean water. Be careful not to feed your hamster too many fatty or sugary treats, as this can lead to health problems.
Finally, you should take your hamster to the vet for regular check-ups. This is especially important for young hamsters, as they may be more likely to develop health problems due to their shorter lifespan. A visit to the vet can help you detect any health issues early and help you to better care for your pet.
Hamster Myths Busted: Separating Fact from Fiction about These Adorable Rodents
There are many myths that circulate about their behavior and needs. However, it’s important for hamster owners to separate fact from fiction to ensure their furry friends stay happy and healthy. One common myth is that hamsters are low-maintenance pets that require minimal care. In reality, these small animals need daily attention, a balanced diet, and a clean living space to thrive.
Another myth is that hamsters are nocturnal and only active at night. While they may be more active during the evening and early morning hours, hamsters are still active throughout the day and require daily exercise and stimulation. By understanding the truth behind common hamster myths, owners can provide their pets with the best possible care and a happy, healthy life.

Adopting a Hamster: What to Know Before Bringing Home Your New Pet.
Adopting a hamster can be an exciting new adventure, but there are a few things to consider before bringing your new pet home. First, make sure you have a suitable habitat set up for your hamster with plenty of space to run and play. Consider the type of hamster you want, as different breeds have varying personalities and care requirements.
It’s also important to find a veterinarian experienced in treating small animals for a checkup and ongoing care. Remember to give your hamster time to adjust to its new surroundings before attempting to handle or play with it, as they can be easily startled. And if you want to give your hamster some extra companionship, consider adopting two of them instead of just one. With proper care and attention, your new hamster can be a beloved and rewarding addition to your household.

Hamster Taming Techniques and Challenges
Hamster Taming Techniques and Challenges can be a rewarding experience for both you and your Hamster. Taming your Hamster takes time, patience, and dedication. Building trust with your Hamster is essential in establishing a good bond with them. To start taming your Hamster, let them get used to their new environment and only touch them while they are in a traveler or a small box. Observe their behavior before you begin the taming session.
Start by feeding them from your hand, which will help them associate your presence with positive experiences. Gradually touch different parts of their body with a brush or your finger, making sure to respect their personal space. Remember that every Hamster has their own unique personality, and the time it takes for them to become tame varies. It’s crucial to earn their trust and never push your Hamster too far too soon. By following these simple techniques, you can build a strong bond with your furry friend and enjoy many happy moments together.

– Hamsters tend to escape from their cages, requiring careful monitoring.
– They have a high tendency to hoard food, making it important to clean out the cage frequently.
Frequently Asked Questions
Should I get my child a hamster?
It is important to consider your child’s age and ability when deciding whether or not to get a pet. Hamsters have an average lifespan of 2-3 years, meaning it will likely be in the family for quite some time. While they are relatively easy to care for, younger children may not be able to provide their necessary daily care and attention. If you have an older child who is capable of providing adequate care, a hamster would make a great companion.
How do I know when my dwarf hamster is in heat?
One way to tell if a dwarf hamster is in heat is to look for signs of behavior changes. During heat, female hamsters may become more active and display increased aggression. Male hamsters may also become more aggressive and display behavior changes such as pacing and mounting.
What makes a better pet a Guinea Pig or a Hamster?
It depends on personal preference, as both guinea pigs and hamsters make great pets. Guinea pigs are typically social and friendly, while hamsters are generally more independent. Both require special care and attention, so it is important to research the specific needs of guinea pigs and hamsters before making a decision.
Do dwarf hamsters prefer to be alone or live with another hamster?
Dwarf hamsters tend to prefer to live with another hamster, but they can live alone if given adequate attention and enrichment.
For a hamster can a deep burrow ever be dangerous?
Yes, a deep burrow can be dangerous for a hamster. If the burrow is too deep, the hamster may become stuck and unable to get out. Additionally, deep burrows could contain predators, parasites, or other dangers that could harm the hamster.
How long does it usually take for a hamster to get used to new owners?
It usually takes a few days to a week for a hamster to get used to new owners.
What does a hamster wheel symbolize?
Hamster wheel symbolism has been prevalent in literature, art, and popular culture. The wheel symbolizes the idea of hope, striving, futility, and the never-ending cycle of life. This can be seen in its use in ancient cultures, where the sun wheel symbolized the eternal cycle of life and nature. In literature, the hamster wheel often represents a character’s struggle with the monotony of life, the inevitability of death, and the cyclical nature of fate.
The wheel also often symbolizes a need for escape from such a mundane existence, as well as a sense of futility in trying to break out of it. The wheel has also come to symbolize freedom, adventure and the possibility of discovery. It is no wonder, then, that the wheel has become such a popular pet icon. Whether taken literally or figuratively, the hamster wheel is a powerful symbol of hope and perseverance, and it is one of the reasons why hamsters make such perfect pets for people of all ages and personalities!
Popular Articles
understanding hamster body language
1. Stretched Out and Relaxed: If your hamster is stretched out and appears relaxed, this is a g…
In The Wild: Exploring The Lives Of Wild Hamsters
In the vast and intricate tapestry of nature, lies a hidden world teeming with life and wonder: the …
Leaky Bladders And Urinary Woes: Understanding Hamster Urinary Issues
They say knowledge is power, and when it comes to understanding the urinary system of our furry frie…
Sleepy Critters: The Wonderful World Of Hamster Napping Habits
In the enchanting realm of sleepy critters, few creatures rival the captivating napping habits of ha…
Unleashing The Dark Side: Inside The World Of Hamster Aggressive Behavior
In the seemingly tranquil and innocent world of hamsters, a darker side exists that is often overloo…
Cash In On Cuteness: Starting Your Own Hamster Breeding Business
In a world where cuteness reigns supreme, there is an opportunity to turn your love for hamsters int…
The Musical Maestros: Decoding The Chirping Hamster Phenomenon
In the fascinating world of hamsters, there exists a perplexing phenomenon that has captured the att…
Heartbreak And Healing: Coping With Hamster Loss Made Easier
In the vast tapestry of life, one cannot escape the threads of heartbreak and loss. The pain we feel…
Out-Of-The-Box Wonders: Unveiling The World Of Creative Hamster Cages
In the world of hamster ownership, a new trend is emerging that challenges traditional notions of wh…
Beyond Pets: Hamsters As Cultural Critters In Modern Society
In the vast tapestry of modern society, where individuals strive for freedom and seek to express the…